AI & Health in China: An Essential Overview
From China's internet hospitals to national healthtech policy engines, this is your field guide to the most advanced health AI ecosystem in the world.
🩺 The Vital Signs series at China Health Pulse provides essential explainers on key contexts and trends shaping health in China today.
My own fascination with AI in healthcare started in the operating theatre.
When I was training in surgery as a resident doctor in the UK’s National Health Service, we were taught the old operating line: See one. Do one. Teach one.
I might have stitched a pork belly once or twice in the lab, but to be honest, that came after I’d already sutured plenty of live patients in theatre. We didn’t practice much on peeling grapes in boxes with keyhole instruments, either. It was straight into real laparoscopic appendicectomies or cholecystectomies, as soon as our seniors gave the nod.
Surgery is an apprenticeship, after all, and there’s truth in the idea that muscle memory builds dexterity and technique. But it cannot be denied that, when so much is at stake, amateur practice on real patients presents questionable odds — even if that has always been the profession’s tradition.
Then the incredible DaVinci surgical robot arrived in our hospital.
It used intelligent robotics to enhance surgeon autonomy, with force feedback systems that let you sense tissue tension with your fingertips, even remotely. We all lined up to try it, and the excitement was palpable among seniors and juniors alike. That machine helped me see clearly: the future of health would be shaped through technology.
Today, I see how AI in health bridges borders to enhance both precision and safety, all around the world: how medical students can practise operations with augmented and virtual reality, getting the reps they need without compromising real patients; how established surgeons outperform their own hands with intelligent robotics, and how experts in New York can remotely operate on patients as far as in India, assisted by real-time AI.
Robotic surgery is just one example of how AI can empower both doctors and patients. Recently, former British PM Tony Blair called for the deployment of “AI doctors” to help fix the NHS, and across London, SF and Boston, every healthtech start-up promises to “revolutionise care” through AI. From my seat on the UK Royal Society of Medicine’s Digital Health Council, I see these promises up close: running national events, curating expert panels and promoting conversations on everything from digital twins to ethical frameworks for remote care.
The innovation is real, and the hype is, too. But after working across both systems, I can say this: China is operating on a different timeline.
Take that same DaVinci robot. Years after I first tried it in the UK, one of my close family members underwent robotic kidney surgery — in China. Its sophisticated functionality allowed part of the kidney to be preserved, instead of having the entire organ removed. Better safety. Better outcomes. Better quality of life. Yet at the time, what was already a widely recognised surgical indication in China, was still used with limitation in UK hospitals.
AI isn’t a future ambition in China. It’s already embedded across every layer of the health system.
China is Already Leading in AI x Health
AI and health in China go far beyond scale and speed. What truly sets it apart is a combination of bold build-out, early integration and a willingness to apply technology directly to systemic problems, with unusual momentum. And that makes it not only worth watching, but essential to understand.
I’ve been tracking this space for years, writing with academics, visiting hospitals, working in big tech, partnering with regulators, and watching with both curiosity and caution, to see where the sharpest edges of AI are being deployed nationally.
I recently wrote how, during visits to Beijing, Shanghai and Hangzhou last month, I saw it all up close: health in China is now digital by default, because life itself has become digital. Where other countries continue proceed with caution, China already integrates. Where others treat “digital health” as a standalone initiative, China now embeds it directly into the operational core of how care is accessed, delivered, and financed.
AI is now well-integrated within China’s public hospitals, community health platforms, and centralised policy infrastructure, but there are still plenty of rough edges. Some tools overpromise. Outcomes vary by region. Regulatory frameworks remain uneven. But the overall direction of travel is unmistakable: from pilot to practice, powered by national mandates, cross-sector partnerships, and a culture of digital fluency among patients, clinicians and administrators alike. My post on the biggest healthcare myths about China I see, provides wider context about trends vs misconceptions.
In November 2024, China’s National Health Commission co-released the “Smart Hospital National Initiative” a comprehensive outline to fully leverage AI's advantages in the healthcare setting. It set clear policy KPIs and covered 84 specific scenarios including medical service management, primary public health services, health industry development, medical education and research, clinical efficiency and workflow metrics, as well as patient satisfaction.
With such strong policy drive, the attraction is clear for industry. Healthcare in China offers both a vast and urgent market and a policy environment that rewards innovation. With an ageing population and increasing demand for chronic disease management, China’s annual healthcare spending could reach an estimated 205 trillion RMB (28 trillion USD) by 2030.
China has become a kind of live experimental lab for health AI, in ways that few other countries can match. That’s why what happens here matters for anyone, anywhere, working in, funding, regulating, or using healthcare.
Below, I break down the five layers where AI is already changing how China delivers health: patient access, clinical practice, hospital operations, community prevention and system governance (scroll to end for summary table).
In future pieces, I will explore each area in more depth, with examples from frontline hospitals, startups and national pilots. But for now, take this as your guide to the basic landscape: what’s already real, where the gaps are, and why the rest of the world should be paying attention now.
To note, this post focuses on how AI is transforming health with direct relation to care systems and patient impact, and not China’s equally impressive biotech pipelines and science-driven R&D. For that, you can read my piece on China’s biotech sector.
1. AI Helps Patients Access Care
In China, healthcare is increasingly seamless, digital and embedded in the platforms people already use daily. I’ve described before how you can simply scan a QR code, input your symptoms and receive guidance via text, voice note, video consult, or book yourself into a public clinic — all at your fingertips.
China’s health AI isn’t a separate app or system. It’s built into social super-apps WeChat and Alipay, which are used for everything from messaging to food delivery, payment, and now, access to care. E-pharmacy orders, insurance claims and doctor follow-ups are all able to happen within the same ecosystem.
Adoption is still strongest in tier 1 and 2 cities, where digital literacy is high and the infrastructure mature, particularly among the tens of millions of younger urban populations. AI is so ubiquitous and invisible that it is no longer labeled as AI by the people who use it every day. It simply is the backbone of how care is accessed at scale:
Symptom checkers integrated into public clinic platforms: Alibaba’s AI Medical Assistant guides users through symptoms and directs them to nearby clinics or online consultations.
Chatbots triaging millions daily via WeChat and Alipay: Baidu’s Melody aims to triage user queries and offer instant recommendations, embedded into platforms patients already use and more discreetly than physical consultations.
“Internet hospitals” as digital front doors: Alibaba, Tencent’s WeDoctor and Ping An Good Doctor are some of the big tech players who have partnered with physical infrastructure to create licensed internet hospitals that enable patients to consult doctors, fill prescriptions, and access follow-up care online, removing the need to physically enter a clinic for first contact.
Why It Matters
Connecting health service delivery with e-prescriptions and online reimbursement or payment provide more than convenience. When so many patients now enter care services through AI-enabled platforms, health systems change from the front door outwards. This all loops back, transforming how people interact with care, how data is generated and how services are designed.
Investors: Massive, sticky platforms with high engagement showcase huge scale, real-world engines for harnessing behavioural data
Biopharma: Valuable channels that can access targeted populations for education, retention and digital trial recruitment
Policymakers: Practical models for managing demand and expanding reach: reducing congestion, expanding access and supporting triage, all without need for costly physical infrastructure
Global health & academia: Real-time population data that provides insights into how digital tools can meet large-scale access needs, applicable for both low and middle income settings
⚠ What to Watch
Digital entry points still exclude key populations. Older adults, rural residents and people with low digital literacy all remain underserved. There’s a lack of standardised validation across platforms, even despite approvals and regulatory scrutiny, and as private firms dominate patient interfaces, accountability for triage outcomes and personal data handling will remain fragmented.
2. AI Helps Doctors to Diagnose and Treat
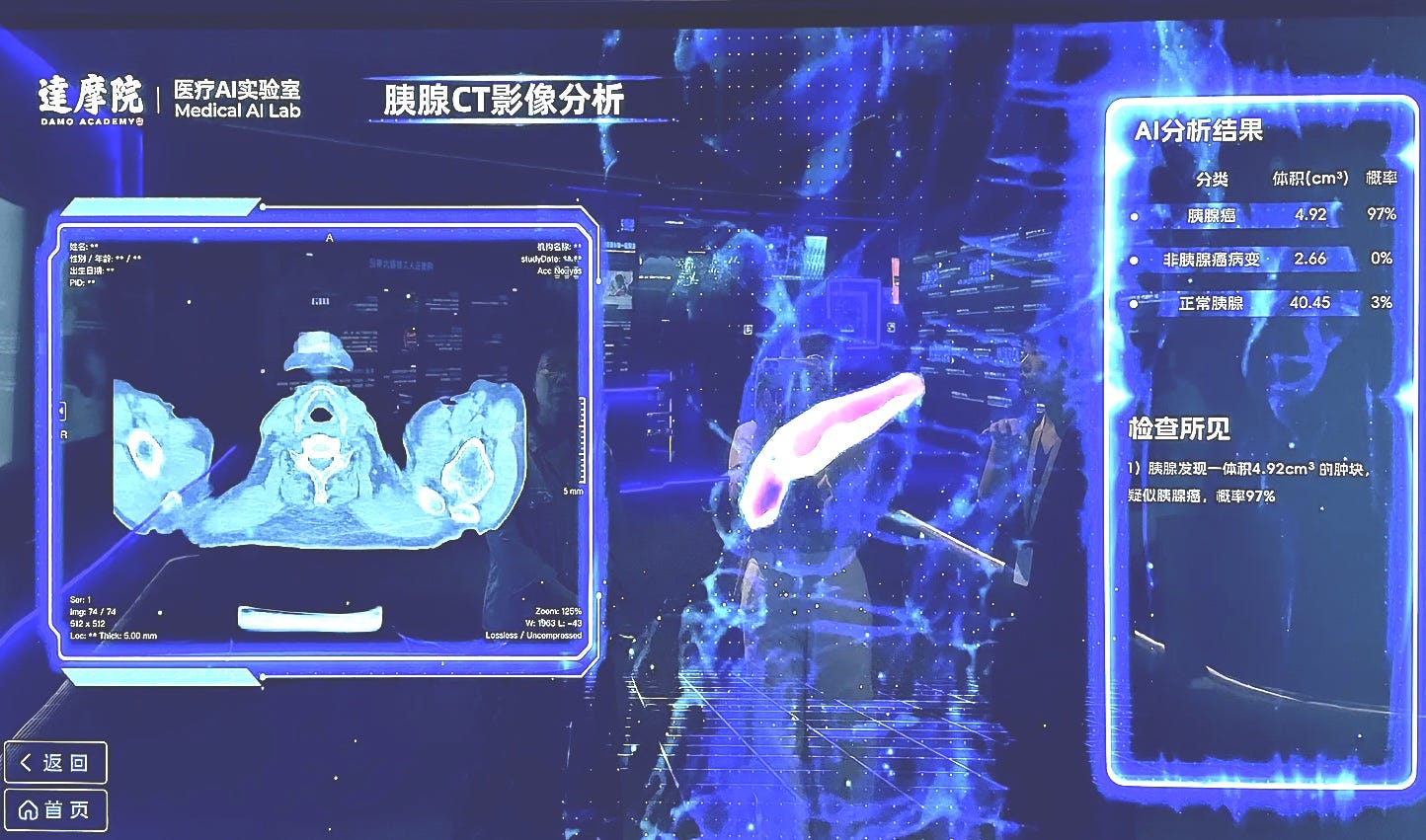
AI is speeding up China’s clinical workflows, standardising quality and expanding access to expertise. Chinese doctors are adopting AI to assist in both diagnostics and therapeutics, including CT scans, X-rays and MRIs to detect benign nodules and cancerous malignancies.
China’s fast AI health uptake can be attributed to the combination of immense disease burden, chronic shortages of trained specialists, and a digital-native policy environment: real pressure and real appetite for diagnostic augmentation. Local companies can access large labeled datasets to tailor real-world tools specifically to Chinese disease patterns:
Diagnostic AI: CT, MRI, ultrasound, and pathology tools are widely deployed across major hospitals. Chinese companies like Mindray already have significant global footprint too, including in the US and Europe.
Therapeutics: In robotic surgery, MicroPort’s SkyWalker system is a Chinese alternative to Da Vinci, used in orthopaedic and laparoscopic procedures.
Clinical decision support: DeepSeek’s AI is already in use in over 100 hospitals, supporting digital nurse triage, medical record summarisation and diagnostic suggestions, including at Peking Union Hospital to diagnose rare diseases through risk stratification and symptom clustering.
Virtual hospitals: Tsinghua’s AIR Agent Hospital is a fully AI-staffed virtual care platform, simulating the entire care journey, from intake to prescription, used for research and potential future clinical deployment.
Why It Matters
AI can super-boost clinical judgment, helping junior doctors make faster, safer decisions, and allowing senior clinicians more time to solve disease complexity. It can scale expertise for overstretched health workforces, without scaling personnel.
Investors: A volume-rich, mission-critical use case that’s already proven in China’s biggest institutions.
Biopharma: Earlier detection means earlier intervention, better trial eligibility and more precise patient identification for targeted therapies.
Policymakers: Supports national goals to improve rural diagnostic quality and standardise care across provinces.
Global health & academia: A testbed to study clinical AI implementation at scale, whether in low-resource or high-volume contexts.
⚠ What to Watch
Not all AI tools are created equal. In lower-tier hospitals, local datasets may be sparse or poorly labeled, which undermines model accuracy. Few systems currently offer clinical audit trails or explainability features. This is a real gap, which complicates trust and safety, as well as responsibility, particularly when AI and human assessments may diverge.
3. AI Helps Hospitals Work Faster
Beyond the patient clinic or doctor’s ward, AI is also reshaping how Chinese hospitals fundamentally function. It can efficiently manage flow, records and decisions, streamlining the behind-the-scenes infrastructure, including for electronic medical records (EMRs), lab results, prescription systems and bed occupancy dashboards, leading to faster triage, safer discharges and smarter staffing:
Ping An Smart Healthcare, AliHealth and Huawei Cloud offer full-stack modular platforms that are integrated into hospital PACS/RIS, EMRs and billing tools. This can include:
Workflow AI: Automates staff scheduling, inventory replenishment and patient routing for efficiency gains.
Smart triage: AI systems pre-sort ED patients, flag high-risk cases and optimise bed assignment.
Real-time dashboards: Used by hospital administrators to monitor bottlenecks, predict discharges and manage clinical KPIs.
Why It Matters
AI can transform through-put, efficiency and patient flow for overstretched public hospitals, as well as optimise service pathways for private health services.
Investors: Recurring SaaS revenue linked to hospital procurement cycles and enterprise-level digitisation.
Biopharma: Better infrastructure provides more reliable real-world data, stronger trial sites and faster recruitment cycles, including valuable feedback loops for monitoring and surveillance.
Policymakers: Eases frontline pressure while meeting performance targets to create more structured, standardised data streams.
Global health & academia: A rare window into what national-scale AI implementation looks like, from initiating procurement to tracking outcomes.
⚠ What to Watch
Hospital-wide systems face practical integration hurdles. Many facilities rely on outdated infrastructure, with fragmented data systems and limited procurement flexibility. Interoperability between platforms remains significantly poor, especially across provinces. This is partly because there are few incentives to share systems, and this will require top-down governance and push. So, while vendor consolidation deepens, the long-term implications for data sovereignty and institutional reliance, are still unfolding.
4. AI Promotes Community Disease Prevention
Prevention is a crucial part of healthcare, that all systems need to focus more on. Delaying or avoiding disease progression at scale is the crucial piece that enables lower costs, smart resource allocation and better patient outcomes. And across China, AI is reshaping how chronic illness is detected, tracked and managed beyond the hospital: in the community, in homes, and through everyday apps and wearable devices.
The stakes are high, and that’s why the AI push is strong. China is ageing rapidly, with rising rates of hypertension, diabetes and cardiovascular conditions. “Healthy China 2030”, the national policy blueprint, has accelerated investments into digital prevention, and tech companies, insurers and local governments have all stepped in:
Wearable-linked risk tracking: Like Apple and Oura’s offers, Huawei and Xiaomi offer popular wearables that monitor sleep, heart rate and so on, with AI-assisted alerts and risk scores.
Digital twins + health scorecards: Ant Group-backed scorecards and Ping An insurer-integrated dashboards simulate patient health states and offer personalised risk reduction prompts.
AI nudges for chronic care: Ping An and regional public health pilots use automated messages to encourage medication adherence, healthy eating and physical activity, especially for diabetes and hypertension.
Home-based monitoring tools: In cities like Shanghai and Hangzhou, pilot schemes link home blood pressure monitors to community clinics via AI-assisted data interpretation.
Why It Matters
China is making keen efforts to decentralise its health approach from frontline of care to daily life, in order to reduce its long-term care burdens. Its experiments provide valuable lessons for other countries facing the same challenges, on what to do, and what not to do.
Investors: Opportunity for markets in ageing tech, digital therapeutics and population risk platforms.
Biopharma: Valuable post-market tracking, digital endpoints and better real-world data.
Policymakers: Supports cost containment and chronic disease control without needing more clinics or staff.
Global health & academia: Offers scalable lessons for other LMICs on prevention tech integration.
⚠ What to Watch
There are hotspots of innovation, and certainly some companies are doing very well, but this health space is consumer-led, and therefore implementation is patchy in terms of both quality and reach. Devices, apps and pilots are all siloed, without needing to adhere too strictly to national data standards. Behavioural nudges often lack long-term validation, and few systems are yet integrated into clinical records, which limit accountability and continuity of care. Uptake again skews younger and urban, while rural communities and older adults remain digitally excluded.
5. AI Powers Health System Governance
Unlike other countries, where governments are often the most resistant to AI adoption, China is already embracing it and eagerly embedding it into national health infrastructure, as both enforcement and optimisation. This is a crucial differentiation that sets China apart from the rest of the world.
From prescription claims to symptom logs, algorithms comb through billions of health transactions, flagging what’s out of line and guiding how public resources are spent. Nearly all drug reimbursements in China flow through the National Healthcare Security Administration (NHSA), and electronic prescriptions are tied to real-name IDs:
Reimbursement and fraud analytics: The NHSA uses AI tools to scan for unusual billing patterns, over-prescription and fraudulent claims
Drug procurement and formulary optimisation: AI tools analyse utilisation patterns and pricing to inform centralised bulk-buying strategies and adjust reimbursement categories in real time.
Outbreak modelling: Provincial CDCs use AI to flag anomalous symptom clusters from outpatient records and pharmacy sales, building early warning systems for infectious disease.
Rare disease identification and registry building: EMRs are mined for diagnostic clues to uncover rare conditions, aiding earlier detection and inclusion in coverage lists.
Why It Matters
In China, AI is operational in public policy. This creates a uniquely centralised health data environment, where system-level view becomes computationally actionable.
Investors: Signals around pricing, reimbursement and market access are increasingly AI-influenced.
Biopharma: AI can determine which products are funded, flagged or excluded, which impact uptake, pricing, and tender dynamics.
Policymakers: Allows real-time surveillance and enforcement without need to expand staff.
Global health & researchers: Useful case studies in algorithm-led governance at the national health system level.
⚠ What to Watch
Despite national ambitions, including by NHSA and China CDC, execution still may vary at the local level, as AI tools are not uniformly implemented across provinces. On the recipient side, patients still lack transparency or consent around how their data is used - even if their concerns might be culturally different from populations in the West. While AI can flag patterns, human oversight and action at the local level still lag, which create gaps between insight and implementation.
To wrap up, for now:
China’s health AI progress matters for all of us. The pressures that drive its domestic adoption (ageing populations, chronic diseases, clinician shortages) are shared by most high-income countries. And as I’ve written before, China’s promises of low-cost, high-volume digital augmentation, hold particular relevance for lower-middle-income countries, whose fewer doctors, fewer hospitals and weaker infrastructure, yet enormous care burdens, have become existential crises.
The open question is whether China’s scale and pragmatism towards AI can translate into global trust. Whether tools trained on Chinese data find traction in African or Southeast Asian contexts. Whether governance models adapt or clash, and if they are implemented abroad, whether they carry intrinsic risks and biases of their own. After all, who gets to define “responsible” use when risks and needs differ so dramatically across geographies and contexts?
This is especially important in healthcare. Compared to other sectors, the stakes are uniquely high for ethical governance: medical records are deeply sensitive, and outcomes can mean life or death. At the same time, the potential upsides are also much clearer in health than almost anywhere else. AI can improve safety, reduce harm and expand capacity, especially in overstretched systems. It can step in where workforces are dwindling, and help clinicians make better decisions in less time.
In future posts on this ever-fascinating topic, I’ll dive deeper into how China’s health AI tools are built, bought and regulated, and where I predict things are heading next.
If there’s a specific angle you’d like me to explore, then as always, I’d love to hear from you.
🩺 The Vital Signs series at China Health Pulse provides essential explainers on key contexts and trends shaping health in China today. Today’s post is an essential overview of AI in healthcare.
For more on China’s healthtech landscape, please see part 1 of my deep dive into Alibaba’s health strategy:
And my essential explainer on the 5 biggest myths in China’s healthcare:






Very valuable information shared in this post. Exciting to know that AI in Health and Robotics industry can help hospitals and doctors to treat patients carefully and avoid medical errors to save life
We are really all so lucky to have you over there on the ground to see what rapid changes are taking place in the Chinese health system, Ruby. As someone who witnessed the change from steam-trains (yes, really, in a small town in lived in the rural south at the turn of the century) to the highspeed trains that traverse the country in a blink of an eye, I'm not surprised to see how rapidly, and apparently seamlessly China has incorporated digital technology in health care. It's great to read how AI can be of useful, practical value - that's where it should be, not in the hands of the techbros who are engaged in industrial level theft of writers and artists work for their own profit. Always fascinating to read your articles Ruby.